Gastroparesis: The Vagus Nerve & Digestion
HOW DOES THE VAGUS NERVE SUPPORT EVERY ASPECT OF DIGESTION?
Your digestive system depends upon the vagus nerve for proper function. Most every aspect of normal digestion, motility (movement of the food/stool) and nutrient absorption depends upon proper vagus nerve function. Without the vagus nerve functioning properly, food and stool does not pass through the intestines normally.
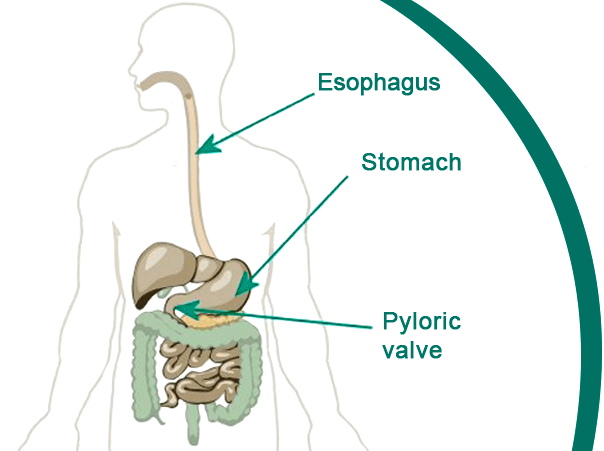
ESOPHAGUS (THROAT)
Your vagus nerve allows proper movement of food down your esophagus toward your stomach. This is called “peristalsis”.
STOMACH
Your vagus nerve triggers your stomach to produce a healthy amount of stomach acid for proper digestion of your food.
PYLORIC VALVE
This valve sits at the base of the stomach and allows food to exit the stomach and move into the intestines. The vagus nerve triggers the opening of the pyloric valve so that food does not sit in the stomach longer than necessary.
GALLBLADDER
The gallbladder stores bile which when released, assists in the proper digestion of food. Gallbladder function is under the control of the vagus nerve (both directly and indirectly).
PANCREAS
The pancreas secretes pancreatic enzymes that assist in digestion and absorption of nutrients, especially fats and proteins. The pancreas is partially controlled by the parasympathetic fibers originating in the dorsal vagal nucleus and the ambiguous nucleus of the brain, then carried by the vagus nerve.
SPHINCTER OF ODDI
The vagus nerve stimulates the Sphincter of Oddi to open, allowing bile (from the gallbladder) and digestive enzymes (from the pancreas) to pass into the intestines.
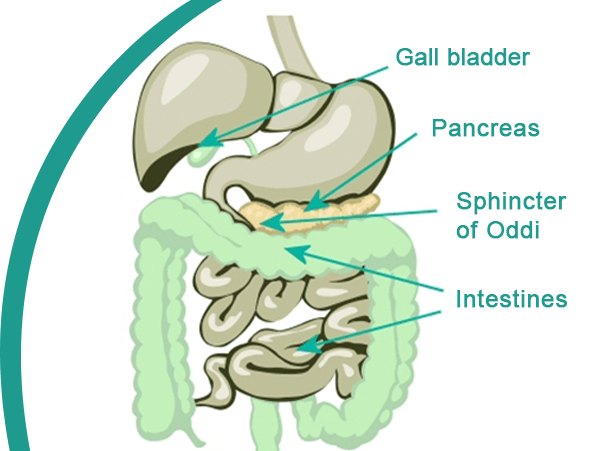
INTESTINES
The vagus nerve stimulates the intestines to push food (or “chime”) along the intestinal tract (“peristalsis”). Proper peristalsis mixes and shifts the chime, allowing proper nutrient absorption. Poor peristalsis can result in gastroparesis, constipation, bloating and discomfort. If partially digested food sits in the intestines without moving, the toxins and free radicals produced are absorbed by the body. The result can be chronic inflammation of the intestinal tract, resulting in poor nutrient absorption, discomfort or pain, and constipation (often alternating with diarrhea).
References
1. Ji H, Rabbi M, Labis B. Central cholinergic activation of a vagus nerve to spleen circuit alleviates experimental colitis. Mucosal Immuol. 2014 Mar :7(2):335-347 2. Parlov VA, Tracey KJ. The vagus nerve and the inflammatory reflex – linking immunity and metabolism. Nature Reviews Endocrinology. 2012; 8:743-754. 3. Borovikova CV, Ivanova S, Zhang M, et al. Vagus nerve stimulation attenuates the systemic inflammatory response to endotoxin. Nature. 2000 May 25; 405 (6785) 458-62. 4. Mukopadhyay AK, Weisbrodt NW. Neural organization of esophageal peristalsis: role of vagus nerve. Gastroenterology. 1975 Mar; 68(3):444-7. 5. Edin R. The vagal control of the pyloric motor function: a physiological and immune histochemical study in cat and man. Acta Physio/Scand Suppl.1980; 485:1-30. 6. Qingfu L, Peng J. Sensory nerves and pancreatitis. Gland Surg. 2014 Nov; 3(4): 284-292. 7. Salvioli B. Bovara M, Barbara G, et al. Neurology and neuropathology of the pancreatic innervation. JOP.2002 Mar; 3(2):26-33. 8. Wood J, Alpers D, Andrews P. Fundamentals of neurogastroenterology. Gut. 1999 Sep; 45 (Suppl 2): 116-1116. 9. Troncom LE, Thompson DG, Ahluwalia NK, etal. Relations between upper abdominal symptoms and gastric distension abnormalities in dysmotility like functional dyspepsia after vagotomy. Gut. 1995 Jul; 37(1):17-22. 10. The NIDDAK Gastroparesis Clinical Research Consortium (6pCRC). Cholecystectomy and Clinical presentation of gastroparesis. Diq DisSci. 2013 Apr; 58(4): 1062-1073. 11. Debas H, Carvajal S. Vagal regulation of acid secretion and gastrin release. Yale Biol Med. 1994 May –Aug; 67(3-4): 145-151. 12. Debas H, Carvajal S. Vagal regulation of acid secretion and gastrin release. Yale Journal of Biology and Medicine. 67(1994), 145-151.
“When I developed gastroparesis, I went everywhere for help but no one could figure out why my gut stopped working! One clue I had was that my gallbladder had also stopped ejecting bile. Because my gallbladder wasn’t filled with gallstones or somehow damaged, I suspected something neurological. Where did I go from there? I will explain what came next in this podcast!”

